Evidence based date wise workflow logs collated by the intern with clickable and verifiable links. Anecdotal self reflections on their internship learning with some video evidence of procedures performed
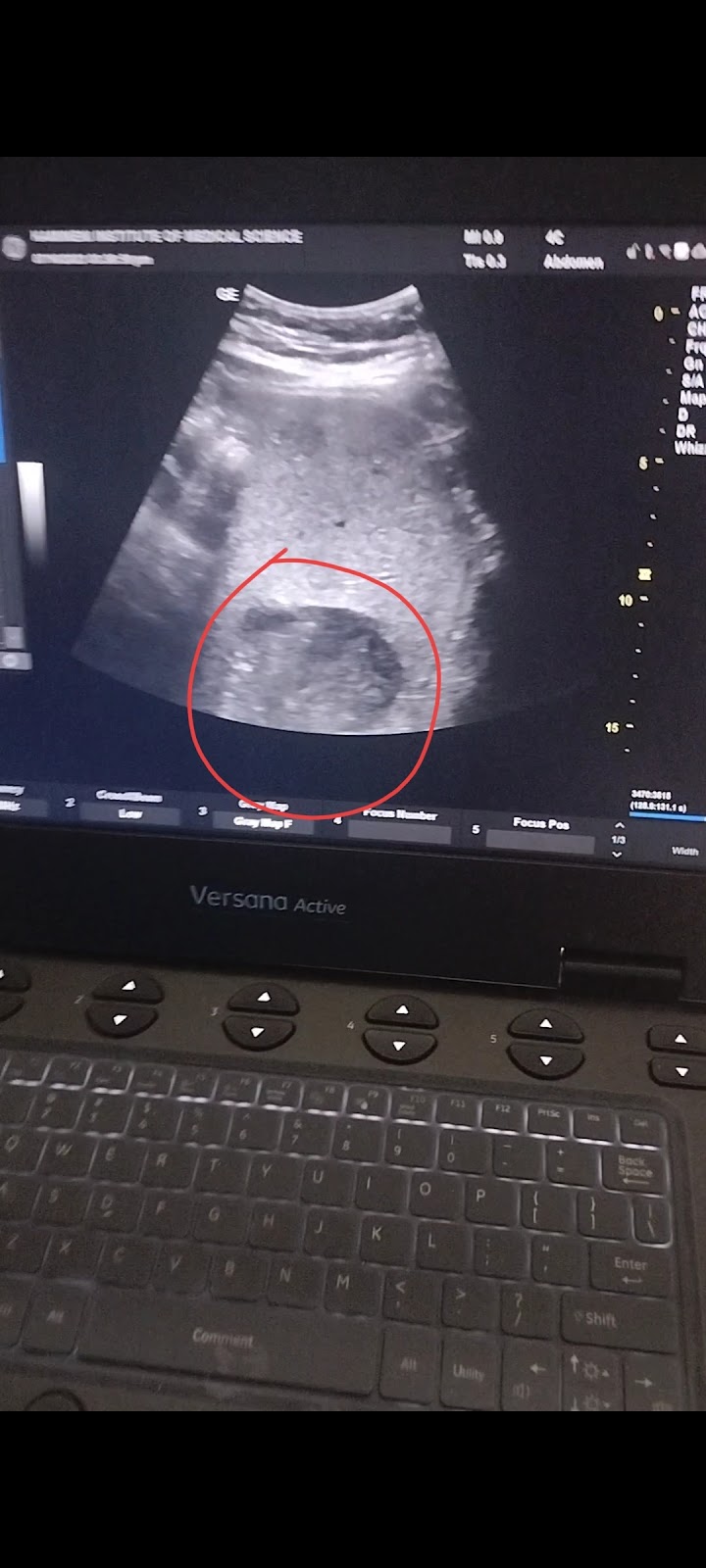
Evidence based date wise workflow logs collated by the intern with clickable and verifiable links. Case 1:- A 32 yr old male came with the complaints of fever since 1 week HOPI Patient was apparently asymptomatic 1 week back and then developed fever which was sudden in onset gradually progressive high grade associated with chills and generalised weakness for which he went to local RMP and took medication for 2 days still the symptoms didnot subside and further investigation like blood test done and his blood sugars were 300mg/dl As the symptoms didnot subside they went to Miryalguda hospital there USG was done and impression showed HEPATIC ABSCESS and refered to our hospital Patient came to hospital yesterday and USG was done impression showing: NO H/o vomitings No h/o cough cold diarrhoea [10/7, 3:08 PM] Rakesh Biswas Sir HOD: Share the ultrasound video or image of his liver abscess asap [10/7, 3:09 PM] Rakesh Biswas Sir HOD: Do the ultra...












Comments
Post a Comment