70 year old male with facial puffiness and lower limb swelling.
- Get link
- X
- Other Apps
A 70 yr old male patient toddy climber by occupation and resident of Nalgonda presented to opd with chief complaints of
Swelling in both legs since 15-20 days
Facial puffiness since 15-20 days.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 3 yrs back. Then he complained of generalized weakness while doing his work which apprently made him discontinue his work.
From past 1 yr he is having constipation 1 episode every 3 -4 days which is occasinally associated with blood which was in minimal quantity. So he visited local doctor with chief complaint of constipation (and he didn't tell about loss of blood in stools back then) . For which the local doctor gave him some medication for constipation which was then temporarily relieved he would have urgency to defecate but would only pass flatus.
There is a history of cough since 4-5 months associated with sputum non blood stained. Excess sputum secretion is present.
He is known to be having intermittent lower leg swelling which would then reduce by itself.
But 20 days back he noticed lower limb swelling upto knees which is pitting type and facial puffiness insidious in onset gradually progressive not associated with chest pain or difficulty in breathing and for which he visited a local rmp for which he was given a tablets and then the edema was subsided temporarily so he went to some other far hospital yesterday where after having his breakfast he alone went to the hospital where he because of travelling and heat he was dizzy and vomited which had food as it's contents non foul smelling non bilious. And after a series of test there he was found to be anemic with hameglobin of 3mg/dl and was referred to higher institution so he came to our opd with cheif complaints of bilater lower limb swelling, facial puffiness and anemia. A 70 yr old male patient toddy climber by occupation and resident of Nalgonda presented to opd with chief complaints of
Swelling in both legs since 15-20 days
Facial puffiness since 15-20 days.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 3 yrs back. Then he complained of generalized weakness while doing his work which apprently made him discontinue his work.
From past 1 yr he is having constipation 1 episode every 3 -4 days which is occasinally associated with blood which was in minimal quantity. So he visited local doctor with chief complaint of constipation (and he didn't tell about loss of blood in stools back then) . For which the local doctor gave him some medication for constipation which was then temporarily relieved he would have urgency to defecate but would only pass flatus.
There is a history of cough since 4-5 months associated with sputum non blood stained. Excess sputum secretion is present.
He is known to be having intermittent lower leg swelling which would then reduce by itself.
But 20 days back he noticed lower limb swelling upto knees which is pitting type and facial puffiness insidious in onset gradually progressive not associated with chest pain or difficulty in breathing and for which he visited a local rmp for which he was given a tablets and then the edema was subsided temporarily so he went to some other far hospital yesterday where after having his breakfast he alone went to the hospital where he because of travelling and heat he was dizzy and vomited which had food as it's contents non foul smelling non bilious. And after a series of test there he was found to be anemic with hameglobin of 3mg/dl and was referred to higher institution so he came to our opd with cheif complaints of bilater lower limb swelling, facial puffiness and anemia.
PAST ILLNESS-
He is known to have fracture on the left lower limb 30 yrs ago.
PERSONAL HISTORY-
Diet Mixed
Appetite Normal
Sleep Adequate
Bladder and bowel Regular
Allergies None
Addictions- Alchohol regular 90 ml
Cigrattes 20 beedis/day since 30 yrs and stopped consuming since a week
FAMILY HISTORY-
No known family history
GENERAL EXAMINATION-
Patient is conscious coherent and co operative well oriented to time place and person.He is moderately built and nourished.
Patient was examined in a well lit room and consent was taken.
Vitals -
PR-78 bpm
BP- 130/80
RR-16cpm
SPo2- 99 ra
Temp-Afebrile
Pallor - present
Icterus - absent
Clubbing - Absent
Cyanosis- Absent
Lymphadenooathy- absent
Edema - bilateral lower limbs till knees pitting type and facial puffiness.
Systemic examination-CVS-
Apical impulse is seen
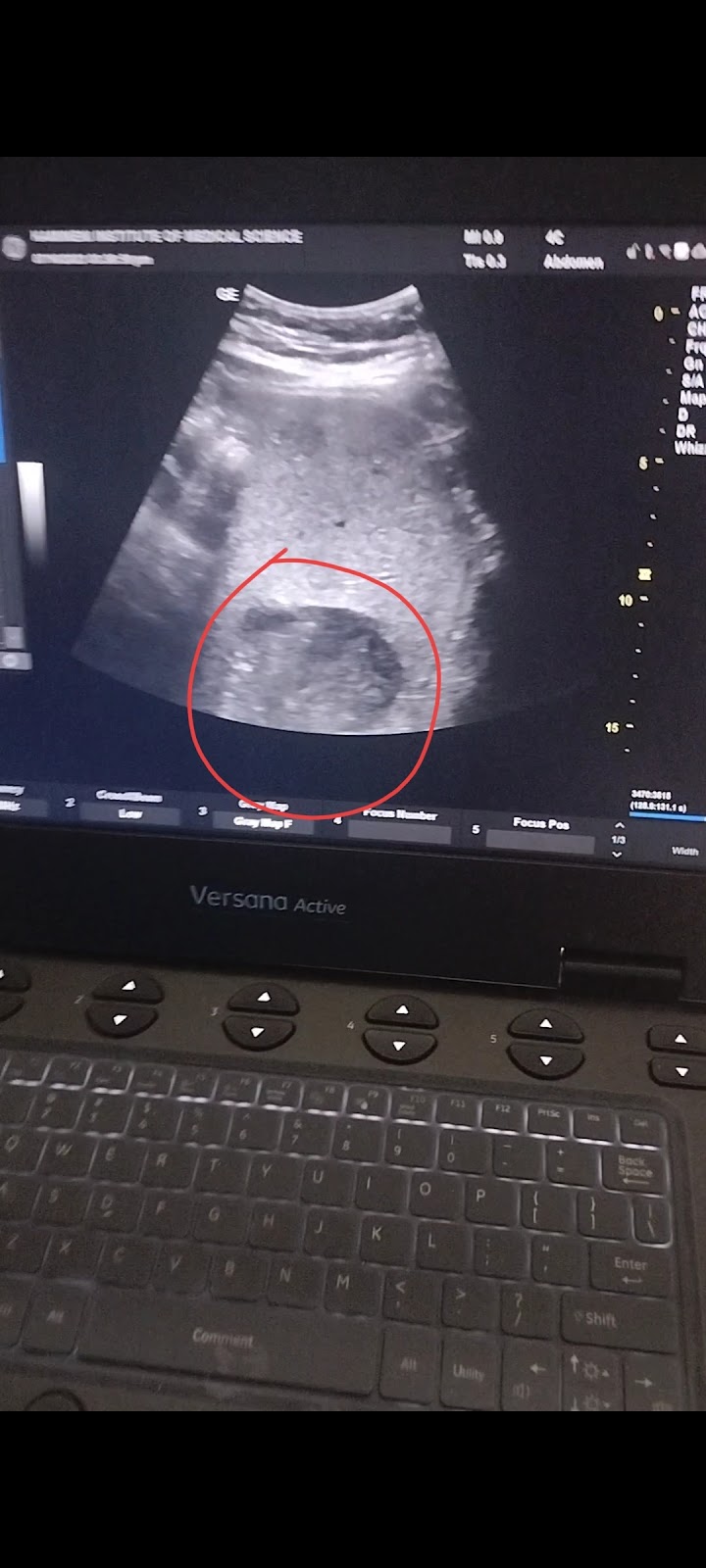
INVESTIGATIONS-
Hameogram-
ECG-Electrolytes-LFT-
CUE-
URINE PROTEIN CREATININE RATIO-
Fever chart-
DIAGNOSIS-
Iron deficiency anemia
? Occasional Bleeding PR
? COPD
- Get link
- X
- Other Apps














Comments
Post a Comment